Cardiovascular System Anatomy & Physiology.
Theheart is the pump responsible for maintaining adequate circulation of oxygenated blood around the vascularnetwork of the body.
... This leads to a 'bottom-up' contraction of the ventricles, forcing blood up and out into the pulmonary artery (right) and aorta (left).

https://www.youtube.com/watch?v=WuBeB7CI6Tc&vl=en
Theheart is the pump responsible for maintaining adequate circulation of oxygenated blood around the vascularnetwork of the body.
... This leads to a 'bottom-up' contraction of the ventricles, forcing blood up and out into the pulmonary artery (right) and aorta (left).
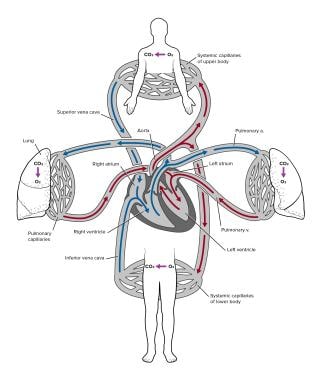
he heart is the pump responsible for maintaining adequate circulation of oxygenated blood around the vascular network of the body. It is a four-chamber pump, with the right side receiving deoxygenated blood from the body at low presure and pumping it to the lungs (the pulmonary circulation) and the left side receiving oxygenated blood from the lungs and pumping it at high pressure around the body (the systemic circulation).
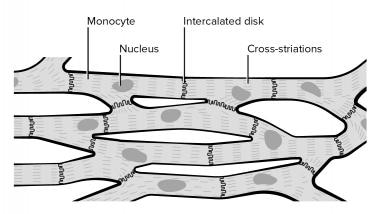
The myocardium (cardiac muscle) is a specialised form of muscle, consisting of individual cells joined by electrical connections. The contraction of each cell is produced by a rise in intracellular calcium concentration leading to spontaneous depolarisation, and as each cell is electrically connected to its neighbour, contraction of one cell leads to a wave of depolarisation and contraction across the myocardium.
This depolarisation and contraction of the heart is controlled by a specialised group of cells localised in the sino-atrial node in the right atrium- the pacemaker cells.
|  |
The 'squeeze' is called systole and normally lasts for about 250ms. The relaxation period, when the atria and ventricles re-fill, is called diastole; the time given for diastole depends on the heart rate.
The ECG
The Electrocardiograph (ECG) is clinically very useful, as it shows the electrical activity within the heart, simply by placing electrodes at various points on the body surface. This enables clinicians to determine the state of the conducting system and of the myocardium itself, as damage to the myocardium alters the way the impulses travel through it.
When looking at an ECG, it is often helpful to remember that an upward deflection on the ECG represents depolarisation moving towards the viewing electrode, and a downward deflection represents depolarisation moving away from the viewing electrode. Below is a normal lead II ECG.
|  |
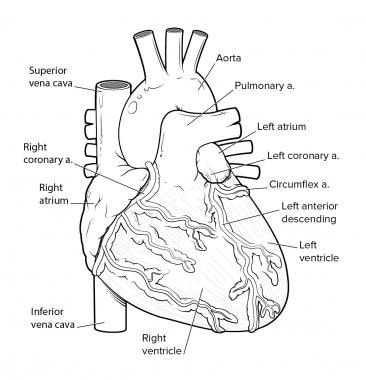
The Coronary Circulation

The heart needs its own reliable blood supply in order to keep beating- the coronary circulation. There are two main coronary arteries, the left and right coronary arteries, and these branch further to form several major branches (see image). The coronary arteries lie in grooves (sulci) running over the surface of the myocardium, covered over by the epicardium, and have many branches which terminate in arterioles supplying the vast capillary network of the myocardium. Even though these vessels have multiple anastomoses, significant obstruction to one or other of the main branches will lead to ischaemia in the area supplied by that branch.
vedio on the link below
Overview
The cardiovascular system consists of the heart, which is an anatomical pump, with its intricate conduits (arteries, veins, and capillaries) that traverse the whole human body carrying blood. The blood contains oxygen, nutrients, wastes, and immune and other functional cells that help provide for homeostasis and basic functions of human cells and organs. [1, 2]
The pumping action of the heart usually maintains a balance between cardiac output and venous return. Cardiac output (CO) is the amount of blood pumped out by each ventricle in one minute. The normal adult blood volume is 5 liters (a little over 1 gallon) and it usually passes through the heart once a minute. Note that cardiac output varies with the demands of the body. [3]
The cardiac cycle refers to events that occur during one heart beat and is split into ventricular systole (contraction/ejection phase) and diastole (relaxation/filling phase). A normal heart rate is approximately 72 beats/minute, and the cardiac cycle spreads over 0.8 seconds. The heart sounds transmitted are due to closing of heart valves, and abnormal heart sounds, called murmurs, usually represent valve incompetency or abnormalities. [4]
Blood is transported through the whole body by a continuum of blood vessels. Arteries are blood vessels that transport blood away from the heart, and veins transport the blood back to the heart. Capillaries carry blood to tissue cells and are the exchange sites of nutrients, gases, wastes, etc. [5]
Gross Anatomy
Heart
The heart is a muscular organ weighing between 250-350 grams located obliquely in the mediastinum. It functions as a pump supplying blood to the body and accepting it in return for transmission to the pulmonary circuit for gas exchange.
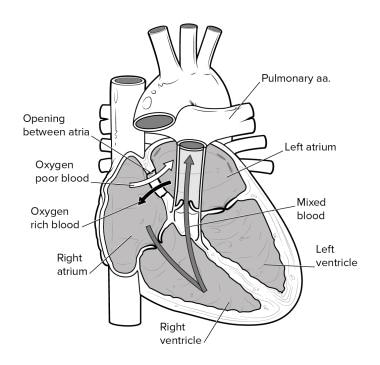
The heart contains 4 chambers that essentially make up 2 sides of 2 chamber (atrium and ventricle) circuits; the left side chambers supply the systemic circulation, and the right side chambers supply the pulmonary circulation. The chambers of each side are separated by an atrioventricular valve (A-V valve). The left-sided chambers are separated by the mitral (bicuspid) valve, and right-sided chambers are divided by the tricuspid valve. Blood flows through the heart in only one direction enforced by a valvular system that regulates opening and closure of valves based on pressure gradients (see image below).
Unique properties of cardiac muscle
Cardiac muscle cells are branching striated, uninucleate (single nucleus) cells that contain myofibrils.
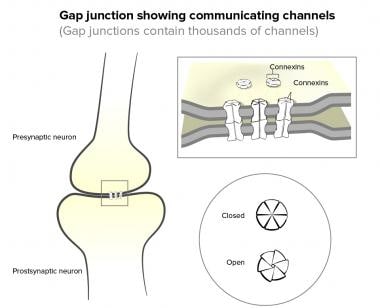
Adjacent cardiac cells are connected by intercalated discs containing desmosomes and gap junctions. The myocardium behaves as a functional syncytium because of electrical coupling action provided by gap junctions.
Cardiac muscle has abundant mitochondria that depend on aerobic respiration primarily to generate adenosine tri-phosphate (ATP), the molecule that provides energy for cellular function (see the images below).
Systemic Circulation
The systemic circuit originates in the left side of the heart and functions by receiving oxygen-laden blood into the left atrium from the lungs and flows one way down into the left ventricle via the mitral valve. From the left ventricle, oxygen rich blood is pumped to all organs of the human body through the aortic semilunar valve (see the image below). [6, 7]
Pulmonary Circulation
The pulmonary circuit is on the right side of the heart and serves the function of gas exchange. Oxygen-poor systemic blood reaches the right atrium via 3 major venous structures: the superior vena cava, inferior vena cava, and coronary sinus. This blood is pumped down to the right ventricle via the tricuspid valve and eventually through the pulmonic valve, leading to the pulmonary trunk that takes the oxygen deprived blood to the lungs for gas exchange. Once gas exchange occurs in the lung tissue, the oxygen-laden blood is carried to the left atrium via the pulmonary veins, hence completing the pulmonary circuit (see the image above).
Coronary Circulation
Coronary circulation is the circulation to the heart organ itself. The right and left coronary arteries branch from the ascending aorta and, through their branches (anterior and posterior interventricular, marginal and circumflex arteries), supply the heart muscle (myocardial) tissue. Venous blood collected by the cardiac veins (great, middle, small, and anterior) flows into the coronary sinus. Delivery of oxygen-rich blood to the myocardial tissue occurs during the heart relaxation phase (see the image below).
Vessel Anatomy
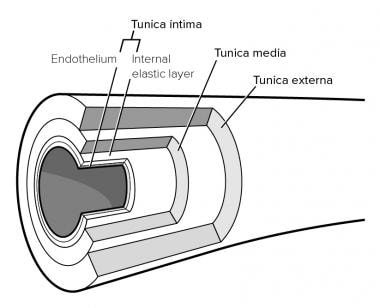
An artery is a blood vessel that carries blood away from the heart to peripheral organs (see the image below). They are subdivided into larger conducting arteries, smaller distributing arteries, and the smallest arteries, known as arterioles, that supply the capillary bed (the site of active tissue cells gas exchange).
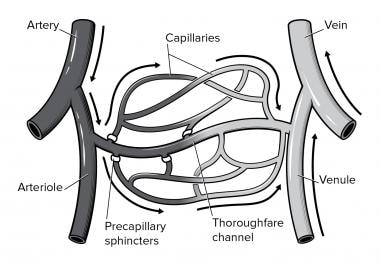
Capillaries are vessels that are microscopic in size and provide a site of gas, ion, nutrient, and cellular exchange between blood and interstitial fluid. They have fenestrations that allow for and enhance permeability for exchange of gas, ion, nutrient, and cellular elements (see the image below).
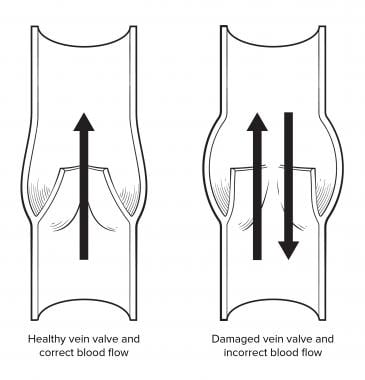
A vein is a blood vessel that has a larger lumen, and sometimes veins serve as blood reservoirs or capacitance vessels, containing valves that prevent backflow. This system of vessels in general returns blood to the heart from the periphery (see the image below).
Natural Variants
Congenital heart anomalies Congenital heart defects cause structural problems of the heart and lead to abnormal or incomplete development of its major chambers and valves, resulting in poor flow and circulation.
Atrial septal defect is a hole in the wall between the right and left atria that promotes mixing of oxygenated and unoxygenated blood. See the image below.
Coarctation of the aorta is a narrowing of the aorta that causes the heart to need to pump harder to force blood through the narrow part of the aorta.
Hypoplastic left heart syndrome is when the left side of the heart does not develop completely, leading to a defective and underdeveloped left ventricle, mitral valve, aortic valve, and aorta.
Atrioventricular canal defect is also known as a endocardial cushion defect and occurs when a hole exists between the chambers of the heart and irregularities with the valves of the heart exist; hence, defects in flow and blood circulation.
Ventricular septal defect is a hole in the septal wall between the right and left ventricles that contributes to the mixing of oxygenated and unoxygenated blood.
Patent ductus arteriosus is a defect in which the connection between the aorta and the pulmonary trunk remains open.
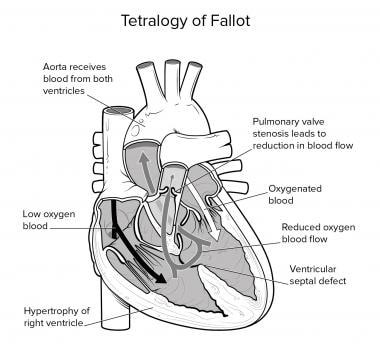
Tetralogy of Fallot is a rare and very serious congenital heart defect involving the heart that includes a stenotic pulmonary valve, an aorta that arises from both ventricles, an interventricular septal opening (ie, ventricular septal defect), and enlarged right ventricle. Babies born with this defect are cyanotic within minutes of birth and require immediate surgical repair. See the image below.
Pathophysiological Variants
Congestive Heart Failure
This is a clinical syndrome that results from the inability of the heart to pump effectively to achieve the cardiac output capable of supplying sufficient oxygen to the peripheral organs for basic metabolic function as well as metabolic demand. Heart failure may be further classified into right ventricular failure, left ventricular failure, or biventricular failure. Some of the main etiologies of congestive heart failure are as follows:
- Cardiomyopathies
- Valvular heart disease
- Systemic hypertension
- Pericardial disease
- Pulmonary arterial hypertension
- High output states such as thyrotoxicosis, anemia or AV fistula.
Cardiomyopathy
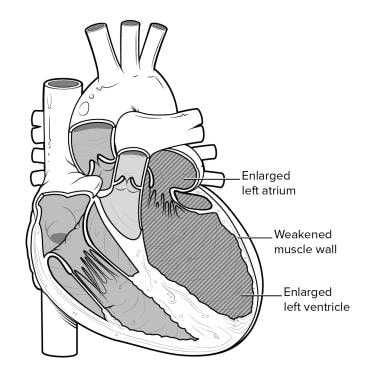
Dilated cardiomyopathy (congestive)
The main characteristic of this condition is a decreased heart contractile function with biventricular dilatation.
The causes may be idiopathic, inflammatory-infectious etiology that may have been caused by postviral myocarditis (coxsackie B or Echo virus), noninfectious etiologies (collagen vascular disease [Lupus, rheumatoid arthritis, polyarteritis]), peripartum, or sarcoidosis.
Toxin induced
Alcohol, chemotherapy agents such as doxorubicin and Adriamycin, drugs such as cocaine, heroin, or organic solvents can cause cardiomyopathy.
Metabolic reasons
Metabolic reasons include hypothyroidism, chronic hypocalcemia, or hypophosphatemia (see the image below).
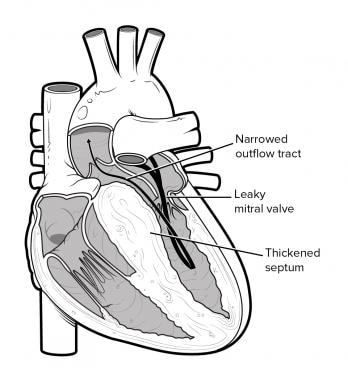
Hypertrophic cardiomyopathy
This condition is caused by a familial autosomal dominant trait resulting in marked hypertrophy of the myocardium and a disproportionate greater thickening of the interventricular septum. This hypertrophied septum can cause narrowing of the sub aortic area due to its opposition to the anterior mitral leaflet resulting in left ventricular outflow obstruction during mid-systole. See the image below.
Restrictive cardiomyopathy
This is characterized by abnormally rigid ventricles that impair diastolic heart filling but the heart retains a normal size and a normal systolic function. A reduced ventricular compliance due to fibrosis or infiltration results in an abnormal high diastolic pressure leading to high systemic and pulmonary venous pressures.
Myocardial fibrosis
Myocardial fibrosis is caused by scarring or infiltration caused by amyloidosis or sarcoidosis; non infiltrative myocardial fibrosis is caused by scleroderma. Other storage diseases such as glycogen storage disease or hemochromatosis may cause this condition.
Endomyocardial fibrosis
Endomyocardial fibrosis is caused by scarring or infiltration caused by hypereosinophilic syndrome and radiation therapy; metastatic tumors may also be considered as other etiologies.
Rheumatic heart disease
Rheumatic heart disease is a serious complication of rheumatic fever. Acute rheumatic fever follows 0.3% of cases of group-A beta-hemolytic streptococcal pharyngitis (a throat infection) in children. Patients with acute rheumatic fever may develop varying degrees of associated valve insufficiency, heart failure, pericarditis, and even death. With chronic rheumatic heart disease, patients develop valve stenosis with varying degrees of regurgitation, atrial dilation, arrhythmias, and ventricular dysfunction. Chronic rheumatic heart disease remains the leading cause of mitral valve stenosis and valve replacement in adults in the United States. Acute rheumatic fever and rheumatic heart disease are thought to result from an autoimmune response, but the exact pathogenesis remains unclear.
Valve conditions
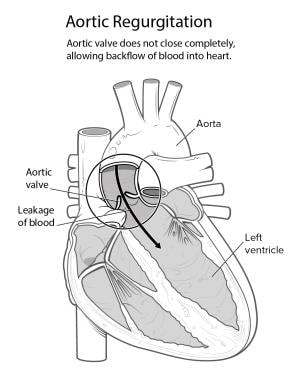
Alterations in the normal functioning of heart valves lead to alterations in the normal cardiovascular physiology. A valve defect may be stenotic or regurgitant. When it is stenotic it represents a valvular opening that is narrowed, thus restricting blood flow through the valve. A regurgitant valve is usually incompetent resulting in back flow through a partially open valve. The atrioventricular valves, mitral valve, and tricuspid valve, prevent backflow into the atria when the ventricles are contracting. The pulmonary and aortic semilunar valves prevent backflow into the ventricles during the relaxation phase.
Mitral stenosis
Mitral stenosis is usually a consequence of rheumatic heart disease. Approximately 50% of those with mitral stenosis usually have a history of rheumatic fever. This can be distinguished by a murmur that is localized near the apex of the heart. See the image below.
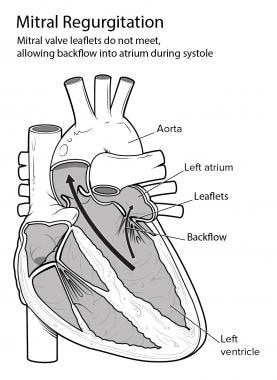
Mitral regurgitation
Mitral regurgitation may result from rheumatic heart disease, mitral prolapse, or ruptured chordae tendineae or papillary muscle dysfunction after a myocardial infarction. See the image below.
Valve defects such as above may be seen clinically as dyspnea on exertion and fatigue like symptoms.
Aortic stenosis
This condition may result from congenital lesions, such as bicuspid aortic valve, rheumatic heart disease, and calcified aortic valve. This can be distinguished by a systolic ejection murmur. [8] See the image below.
Aortic regurgitation
This condition may be a result of rheumatic heart disease, endocarditis, valvular congenital structural heart defects, syphilis or aneurysms. Aortic valve defects may be seen clinically presenting with signs or symptoms of congestive heart failure, angina, syncope or decreases in exercise tolerance. See the image below.
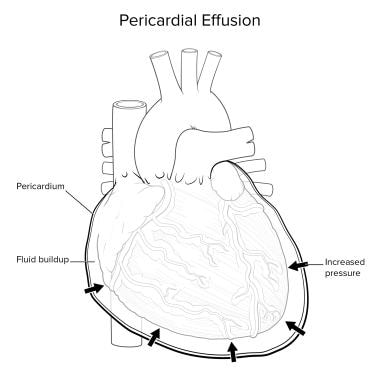
Pericarditis
The heart is surrounded by a sac of tissue known as the pericardium that functions as a protective layer to the heart and also reduces friction with adjacent organs. Inflammation of this layer is known as pericarditis. The clinical manifestations of acute pericarditis are due to the inflammation of the pericardium; treatment is targeted with anti-inflammatories such as aspirin or NSAIDs, while the clinical manifestations of chronic pericarditis are usually due to the constriction of pericardium around the myocardium. Because the right ventricle operates under lower pressures than the left ventricle, the right ventricle is primarily affected by the constricted pericardium. Constrictive pericarditis usually presents with right-sided symptoms because the right ventricle does not fill with normal capacity due to the anatomic bottleneck caused by the constricted pericardium, hence causing venous congestion, preload reduction, and a reduction in cardiac output. Pericarditis has multiple causes, asfollows:
- Infectious etiologies include viral (coxsackie B), bacterial, tuberculosis, fungal, amoebic, and protozoan.
- Rheumatologic etiologies include systemic lupus erythematosus, rheumatoid arthritis, mixed connective tissue disorder, and scleroderma.
- Post mediastinal radiation secondary to radiation therapy for malignancy, such as breast cancer, lymphoma, and lung cancer.
- Uremia: Kidney failure may be a cause for a metabolic abnormality leading to pericarditis.
- Trauma: Either blunt for sharp injury to the chest, cardiac procedures that are invasive, or post myocardial infarction are possible causes.
- Medications: A number of drugs may cause pericarditis, such as penicillin, cromolyn sodium, doxorubicin, cyclophosphamide, procainamide, hydralazine, methyldopa, isoniazid, mesalazine, reserpine, methysergide, dantrolene, minoxidil, and phenytoin.
- Gastrointestinal: Patients with inflammatory bowel disease such as Crohn disease or ulcerative colitis may develop pericarditis as a consequence.
- Undetermined or idiopathic: Treatment is targeted at the cause as well as toward any complication such as pericardial effusion (see image below) where an effusion at the pericardial sac causes anatomic pressure around the heart, restricting its ability to relax and pump with adequate pressures. The treatment for pericardial effusion is pericardiocentesis, in which a needle is inserted to drain the excess pericardial fluid, thus relieving the external pressure.
Systemic Hypertension
Blood pressure is influenced by cardiac output, peripheral resistance of vessels, and blood volume. Vessel diameter is the most important of these factors, and small changes in vessel diameter significantly affect blood pressure. Blood pressure varies directly with both cardiac output and blood volume; it varies inversely with vessel diameter. Blood pressure is regulated by autonomic neural reflexes involving baroreceptors, chemoreceptors, the vasomotor center, and vasomotor fibers acting on vascular smooth muscle inputs from higher central nervous system centers, chemicals such as hormones and renal compensatory pathways. Blood pressure above the normal ranges of 120 mmHg systolic and 80 mmHg diastolic are considered prehypertensive (120-139/80-89) mmHg. Stage 1 hypertension is defined as blood pressure of 140-159/90-99 mmHg. Stage 2 hypertension is defined as blood pressure greater than 160/greater than 100 mmHg. The most common type of hypertension isessentialhypertension ,for which the cause is unknown. This accounts for up to 98% of patients. The remaining 2% have secondary causes, such as renal disease, pheochromocytoma, mineralocorticoid excess, aortic coarctation, or pre-eclampsia during pregnancy. Malignant hypertension is when the blood pressure is greater than 200 systolic and 140 diastolic with evidence of papilledema. This is a medical emergency, and the blood pressure must be controlled adequately and promptly.
Other Common Abnormal Cardiovascular Conditions
Angina pectoris
This is the clinical syndrome that occurs when heart oxygen demand exceeds blood supply resulting in pain or discomfort in the chest and adjacent areas. Angina may be classified as stable or unstable. This condition may result from myocardial ischemia that is a result of a reduction in coronary blood flow caused by a fixed or dynamic coronary artery blockage, an abnormal constriction or decreased relaxation of the coronary microcirculation, or a reduction in the oxygen-carrying capacity of the blood.
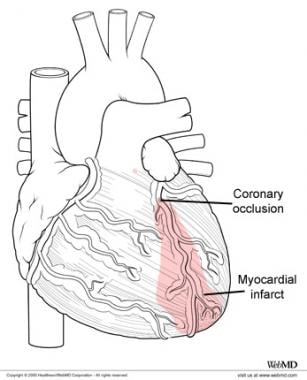
Myocardial infarction
Myocardial infarction is a condition in which the heart muscle is damaged due to lack of blood supply or ischemia in the coronary vessels and, thus, the heart is unable to pump blood effectively to the peripheral organs. Atherosclerosis is the most common cause of coronary artery stenosis resulting in myocardial ischemia. The infarction area or area of ischemia is isolated to the muscular area of blood supply resulting in poor or lack of function of that regional area of heart muscle. For example, a blockage in the left circumflex artery may result in damage to the left ventricular muscle; likewise, a right coronary artery defect or ischemia may result in right heart ventricular dysfunction. See the image below and the area of heart blood supply versus regional infarcted area.
for the gallary media click below link for the photos attached here
https://emedicine.medscape.com/article/1948510-overview#a4



My husband was diagnosed with early onset Parkinson's disease at 57.his symptoms were shuffling of feet,slurred speech, low volume speech, degradation of hand writing, horrible driving skills, right arm held at 45 degree angle, things were tough for me, but now he finally free from the disease with the help of total cure ultimate health home, he now walks properly and all symptoms has reversed, he had trouble with balance especially at night, getting into the shower and exiting it is difficult,getting into bed is also another thing he finds impossible.we had to find a better solution for his condition which has really helped him a lot,the biggest helped we had was ultimatehealthhome they walked us through the proper steps,am highly recommended this ultimatehealthhome@gmail.com to anyone who needs help.
ReplyDelete